Pain in the anterior tibial tendon is a common condition, especially in active individuals, runners, or patients with postural or gait abnormalities.
In many cases, this pain is accompanied by decreased activation of the anterior tibialis, which can impair function and lead to chronic symptoms.
However, not all activation deficits have the same origin. Some stem from central activation issues, while others are related to errors in movement execution.
If you work with patients who show signs of reduced muscle activation, understanding the true origin of the problem is key to guiding treatment.
Thanks to EMG with biofeedback, it’s now possible to identify whether the deficit is central or mechanical—allowing you to make more precise clinical decisions and retrain muscle patterns objectively and efficiently.
👉 Discover how mDurance EMG can help improve your patients’ muscle activation from day one.
In this post, you’ll learn how to differentiate between these two types of deficits using real examples—and how to apply tools like surface EMG and biofeedback to effectively retrain muscle function and movement.
Step 1: Evaluate Muscle Activity with an Isolated Test
The first step is to assess whether there’s a real muscle deficit in the anterior tibialis. For this, we use a simple test: manually resisted dorsiflexion.
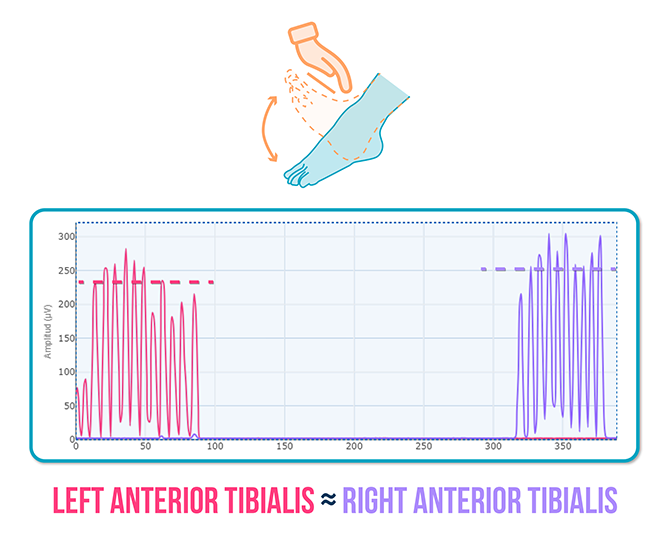
Right anterior tibialis = Left anterior tibialis
✅ This indicates there’s no central deficit, as the muscle is able to activate normally when isolated in a specific voluntary contraction.
Step 2: Assess a Functional, Loaded Movement
Next, we analyze muscle activity during a more complex movement: the squat, which involves motor control, stability, and coordination.
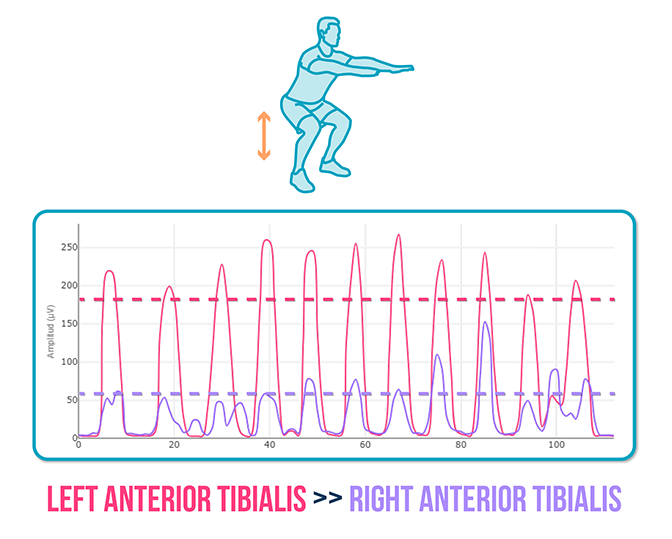
Right anterior tibialis << Left anterior tibialis
❌ Although both muscles activated equally in the isolated test, during the squat the right anterior tibialis showed much lower activation, suggesting a mechanical dysfunction likely related to the motor pattern.
So Where Was the Problem Really?
Even though the right anterior tibialis showed similar activation to the left in the analytical evaluation, during a functional task like a squat, its activation was clearly reduced.
This discrepancy isn’t due to a structural muscle deficit, but rather to how the muscle integrates into the loaded motor pattern.
Specifically, the issue arose when the foot was in contact with the ground—acting as a fixed distal point.
In this situation, which requires stabilization and load control, the right anterior tibialis failed to activate as effectively as the healthy side.
This leads us to conclude that the problem wasn’t the muscle itself, but an altered neuromuscular integration of the anterior tibialis within the functional movement pattern.
In other words, the muscle wasn’t activating properly when the system required its participation to stabilize the joint during the squat.
To address this altered pattern, we used a key tool: EMG biofeedback, allowing the patient to see their muscle activation in real time and adjust their execution accordingly.
Biofeedback Reeducation: Two Strategies in Action
First Strategy: Biofeedback with Simple Instruction
The patient was instructed to “raise the purple line,” corresponding to the right anterior tibialis on the EMG graph.
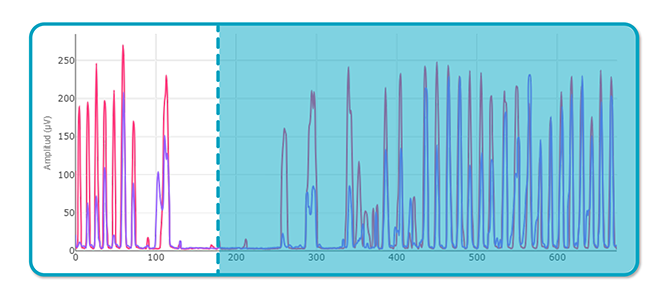
❌ Result:
– The patient was unable to increase muscle activation.
– A verbal cue alone wasn’t enough to modify the motor pattern.
Second Strategy: Biofeedback + Detailed Explanation
This time, the feedback was accompanied by a more specific instruction:
“Try to place your entire foot down, including the heel—not just the midfoot—and aim to raise the purple line.”
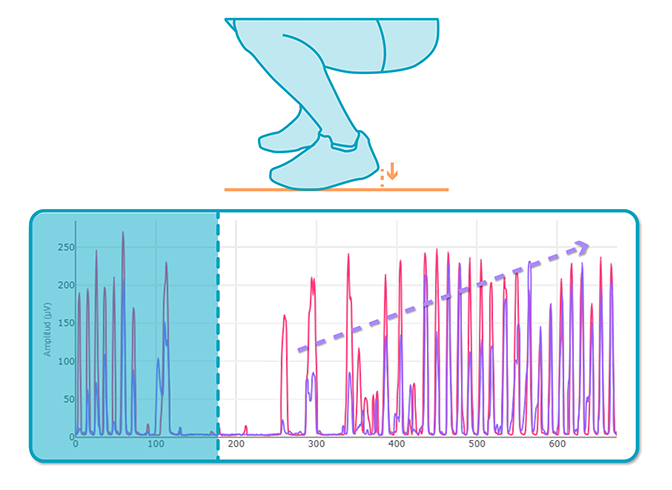
✅ Result:
The patient successfully increased right anterior tibialis activation, corrected squat execution, and adjusted their motor pattern thanks to the combination of visual and verbal feedback.
Comparing the EMG graphs clearly shows how using biofeedback along with a detailed explanation led to a significant improvement in muscle activation.
The patient went from a dysfunctional to a more efficient pattern—not by increasing muscle strength, but by correcting how he moved.
Key Takeaways
This case highlights a crucial insight:
Not all activation deficits are due to muscle activation issues. Sometimes the problem lies in the movement, not the muscle.
Using tools like EMG with biofeedback allows you to:
- Identify whether a deficit is central or mechanical.
- Make more precise clinical decisions.
- Retrain muscle activation in an effective and objective way.
If you want to improve how your patients activate their muscles during movement, surface EMG from mDurance is your ally.
👉 Contact us and discover how to enhance your assessments and treatments with EMG.
See you in the next post 🙂