Case Study: EMG-Guided Rehabilitation
Sensory-motor denervation is one of the greatest challenges in neuromuscular physiotherapy. When the connection between the nervous system and the muscle is affected, recovery depends not only on strength, but on teaching the muscle how to activate again.
Applying the same standard exercise program you would use with any patient is a mistake. This can completely stall progress.
Why? Because the affected muscle doesn’t always respond to expected stimuli, and without objective measurement, you can’t know if it’s actually participating in the movement.
Surface electromyography (sEMG) allows you to see in real time whether the muscle activates, how much it does, and how it changes with each exercise. This completely transforms how you approach rehabilitation.
👉 Want to integrate EMG into your rehabilitation protocols and design truly personalized treatments?
Contact us here and we’ll give you a private walkthrough of our EMG system.
Challenges in Patients With Denervation
In a patient with medial gastrocnemius denervation, the main difficulties you’ll encounter are:
- Minimal or absent activation during conventional exercises.
- Automatic compensations from other muscles (like the lateral gastrocnemius or soleus).
- Progressive loss of strength and tone due to ineffective neural stimulation.
And the big question in clinic is:
“How can I tell if the exercise I’m using is actually activating the affected muscle?”
The only way to answer that with certainty is to measure muscle activity directly.
Initial Assessment: Muscle Analysis With EMG
We began the session with a simple test: bilateral heel raises.
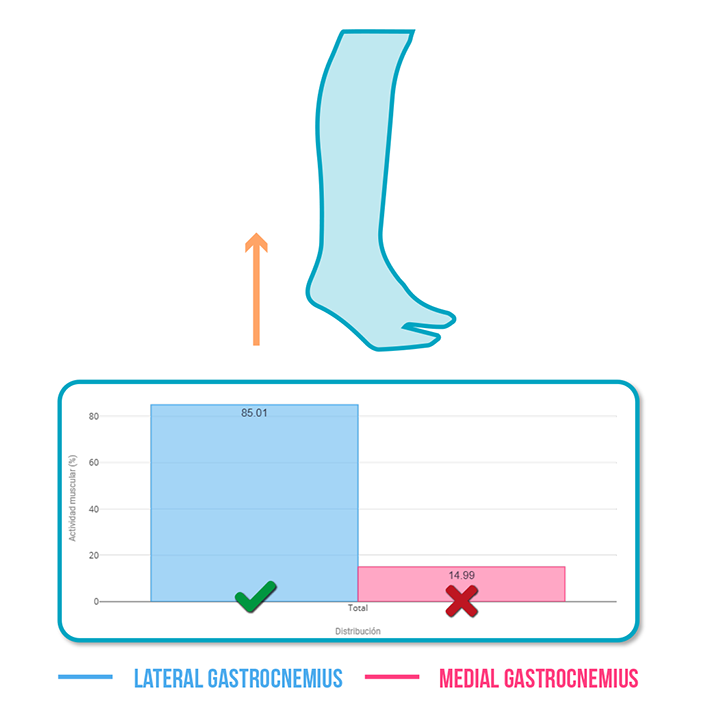
EMG results:✅ Lateral gastrocnemius: 27% mean activation
❌ Medial gastrocnemius: 14.9% mean activation
This revealed a motor asymmetry greater than 70%, confirming the lack of effective activation in the medial gastrocnemius.Initial conclusion: The muscle was not responding to the usual motor pattern — a more specific stimulus was needed.
Strategy: Find the Exercise That Best Reactivates the Medial Gastrocnemius
The next step was to test different variations of the same movement to identify which one improved neuromuscular response in the affected calf.
The goal was to elicit a stronger, more efficient electrical signal.
Exercise 1: Asymmetric Heel Raise With Hands Supported on a Box
EMG results:
✅ Medial gastrocnemius activation increased by 5% compared to the initial bilateral test.
Interpretation: Partial support allowed greater neural focus on the affected leg, reducing compensation from the healthy side.
Exercise 2: Assisted Asymmetric Heel Raise With TRX
EMG results:
✅ 8% increase in medial gastrocnemius activation.
Interpretation: The TRX improved stability and control, enabling reactivation without excessive fatigue.
Exercise 3: Asymmetric Heel Raise With Manual Support and 4 kg Load
EMG results:
✅ Additional 8% increase in medial gastrocnemius activation compared to the TRX exercise.
Interpretation: Activation of the medial gastrocnemius progressively normalized, reducing the difference with the lateral head.
The Key: Personalization Through EMG
Each patient with denervation requires a tailored activation protocol. EMG helps you design that protocol based on real data, not assumptions.
With EMG, you can:✅ Select the most effective exercise to stimulate the denervated muscle.
✅ Detect and avoid compensations by other muscles.
✅ Use real-time biofeedback to teach the patient proper activation.
✅ Motivate the patient with visible, measurable progress.
Clinical Implications
Without EMG, this case could have been mistaken for a simple strength deficit. However, the recordings revealed the true issue: a neuromuscular problem, not a structural one.
This completely changed the treatment approach, from generic strengthening to data-driven motor reeducation.
The result was a progressive, measurable improvement in medial gastrocnemius activation, marking a turning point in the patient’s recovery.
Conclusions
Not every exercise works for every patient. In cases of denervation or neuromuscular deficit, precision makes the difference between progress and stagnation.
Surface EMG lets you see what the eye can’t measure: Which muscles activate, how strongly they do, and how they respond to every exercise modification.
See you in the next post 🙂