Imagine a patient comes to your clinic with recurrent knee pain. You’ve tried different treatments, but the issue persists. What if the root cause isn’t where it seems?
Without an objective evaluation of muscle function, it’s easy to overlook imbalances, inhibitions, or compensations that may be affecting movement and prolonging the problem.
Surface Electromyography (EMG) allows you to see in real-time how muscles function, identifying whether they are activating correctly or if there is an underlying issue. With this information, you can design a more precise and effective treatment.
In this post, you will learn the three essential steps to assess muscle function and determine whether it falls within normal parameters or presents alterations. This will help you make better clinical decisions and improve communication with your patients.
Step 1 – Bilateral Comparison
The first step in evaluating muscle function is to compare activity between the healthy and affected sides. This comparison helps detect asymmetries that may indicate compensations, weaknesses, or neuromuscular response alterations.
Why is this important?
A muscle that should activate similarly on both sides but shows reduced activation on the affected side may be inhibited or functioning inefficiently.
This is often a primary cause of movement dysfunctions, increased strain on other structures, and prolonged recovery time.
Practical Example:
A patient with supraspinatus tendinopathy in the right shoulder performs an external rotation exercise without abduction.
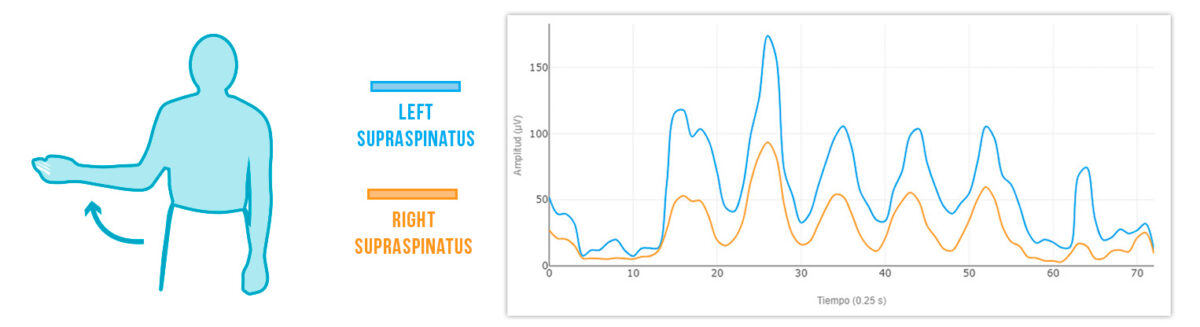
By analyzing muscle activity with EMG, you observe that the right supraspinatus (yellow line) shows a deficit in activation, while the left side functions normally.
This information allows you to adapt the treatment to properly activate the affected muscle and prevent compensations that could worsen the condition.
Step 2: Evaluating the Synergy Between Agonist, Synergist, and Antagonist Muscles
It’s not enough to know if a muscle is activating or not; it’s also essential to understand how different muscle groups work together. In this step, analyze the relationship between agonists, synergists, and antagonists to check if the activation pattern is optimal.
Why is this important?
If an agonist muscle is underactive or if an antagonist muscle is overactive, movement can be altered, leading to compensations, overload, and potential injuries. EMG evaluation of muscle synergy allows you to identify and correct these imbalances.
How to do it:
- 1. Define which muscles should activate more (agonists) and which should activate less (antagonists) for the movement being evaluated.
- 2. Analyze the EMG data to verify if the activation follows the expected pattern.
- 3. Adjust the treatment strategy based on your findings.
💡 Tip: mDurance provides the most comprehensive synergy guide to help you interpret these data and optimize your analysis.
Practical Example:
A patient comes to the clinic with left shoulder pain. To evaluate their muscle function, you assess shoulder abduction and analyze supraspinatus and upper trapezius activation with EMG.
In a normal activation pattern:
Supraspinatus should activate more than the upper trapezius:
Supraspinatus > Upper Trapezius
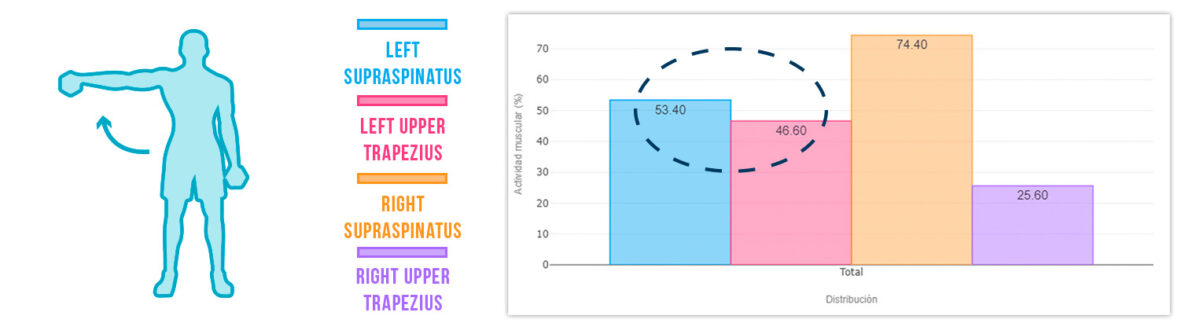
However, in this case, you observe:
🔹 Left supraspinatus → Activation deficit ❌
🔹 Left upper trapezius → Overactivation ⚠️
This imbalance suggests that the supraspinatus is not working properly, forcing the upper trapezius to compensate excessively.
Identifying this alteration allows you to adjust the treatment to reduce trapezius overload and enhance supraspinatus activation, preventing the issue from becoming chronic.
Step 3: Analysis Based on Clinical Experience
EMG provides objective data, but the interpretation of that data is key to an effective evaluation. This is where your clinical experience plays a fundamental role. Comparing results with previous patterns and similar cases helps you detect alterations more quickly and accurately.
Why is this important?
Muscle activation values vary between individuals, so there isn’t always a universal threshold to determine if a muscle is functioning correctly.However, with practice and comparison to other cases, you can develop a strong clinical criterion to improve decision-making.
Practical Example:
A patient with low back pain performs a hip extension exercise.
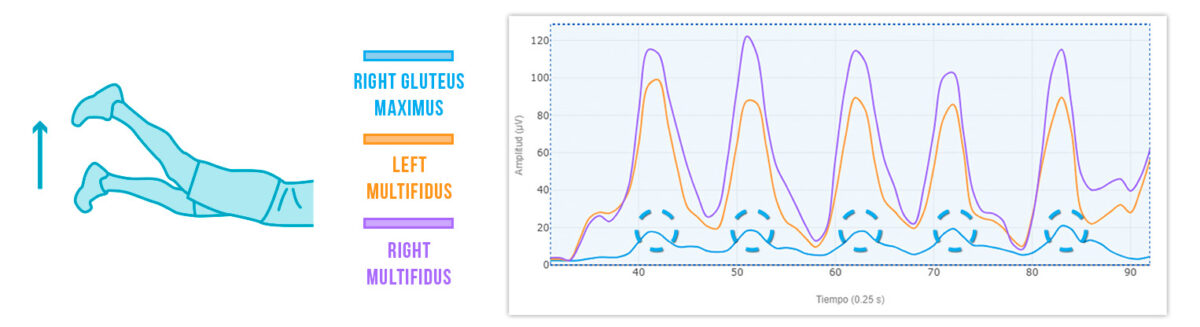
By analyzing EMG data, you observe that the gluteus maximus peaks at only 20 µV, a significantly low value compared to expected levels. Keep in mind that baseline muscle activation in a resting state ranges between 5-30 µV.
This means you have identified a gluteus maximus activation deficit ❌This result, combined with your clinical experience, confirms that the gluteus is not activating correctly, which could be contributing to the patient’s low back pain. With this information, you can adjust treatment to improve glute activation and reduce strain on other structures.
Conclusion
Detecting alterations in muscle function is essential for optimizing patient recovery. By following these three essential steps—bilateral comparison, muscle synergy analysis, and clinical experience application—you can achieve a more accurate evaluation and make better therapeutic decisions.
EMG provides objective data that complement your clinical assessment, allowing you to identify activation deficits, compensations, and muscle imbalances with greater reliability.
Integrating EMG into your practice helps you personalize treatments, avoiding assumption-based approaches and ensuring that each intervention addresses the patient’s true functional state. With a detailed evaluation, you can correct inadequate activation patterns, prevent injuries, and accelerate recovery, ultimately improving the effectiveness of your therapy.