Many professionals struggle to determine the underlying cause of their patients’ lower back pain due to its multifactorial nature.
An evaluation or treatment that does not consider the complexity of neuromuscular variables leads to incomplete or inaccurate diagnoses. For example, a patient may report acute lower back pain after a seemingly harmless exercise routine, without a specific event triggering the pain. This scenario can be confusing and may lead to treatments that temporarily relieve symptoms without addressing the root cause.
If not properly identified and treated, neuromuscular imbalances that contribute to lower back pain can lead to long-term issues, such as the reinforcement of compensatory motor patterns, reduced mobility, and an increased risk of recurrent injuries.
These problems not only affect the patient’s quality of life but also negatively impact their perception of physiotherapy’s effectiveness, resulting in decreased treatment adherence.
In this post, we will break down five key neuromuscular variables that may contribute to your patients’ lower back pain. You’ll gain a deeper understanding of how to address this condition at its root.
Using Electromyography to Understand Lower Back Pain
When dealing with lower back pain, one of the biggest challenges is identifying which muscles are contributing to the problem. Is it a matter of weak muscles not doing their job, or is it an overcompensation that leads to fatigue and muscle stress? This is where EMG provides answers.
Surface electromyography allows you to see real-time activity of the muscles you are evaluating.
Instead of relying solely on interpreting the patient’s pain or symptom descriptions, you obtain concrete data showing which muscles are active when they shouldn’t be, or if they are insufficiently active during specific movements.
Imagine working with a patient who has not made significant progress in their lower back pain treatment. With EMG, you might discover that their lumbar muscles are constantly tense, even at rest, or that their core stabilizers are not activating properly during basic activities.
This information allows you to adjust and personalize treatment, focusing on strengthening underactive muscles and teaching the patient to relax those that are chronically tense.
Now, let’s break down the five key variables contributing to your patient’s lower back pain:
5 Key Neuromuscular Variables Contributing to Lower Back Pain
1. Muscle Imbalances Between Trunk and Hip Agonists and Antagonists
You can identify whether there is excessive or insufficient activity in certain muscle groups, such as the spinal erectors, multifidus, obliques, and glutes.
For example, take a look at how a patient’s muscles activate during a glute bridge:
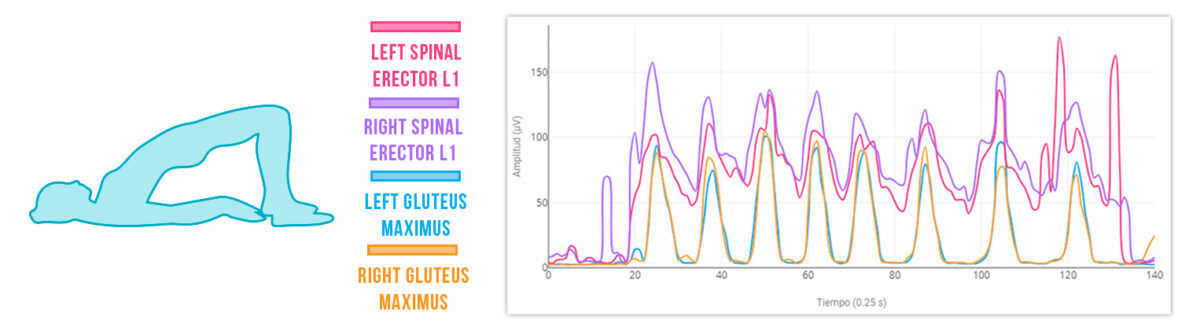
Spinal erectors show higher activity than the glutes, generating a continuous compensatory pattern during the exercise.
2. Overuse or Fatigue of Lumbar Muscles
EMG can reveal signs of muscle fatigue during repetitive movements and tasks. Check out the activation results for this patient while running:
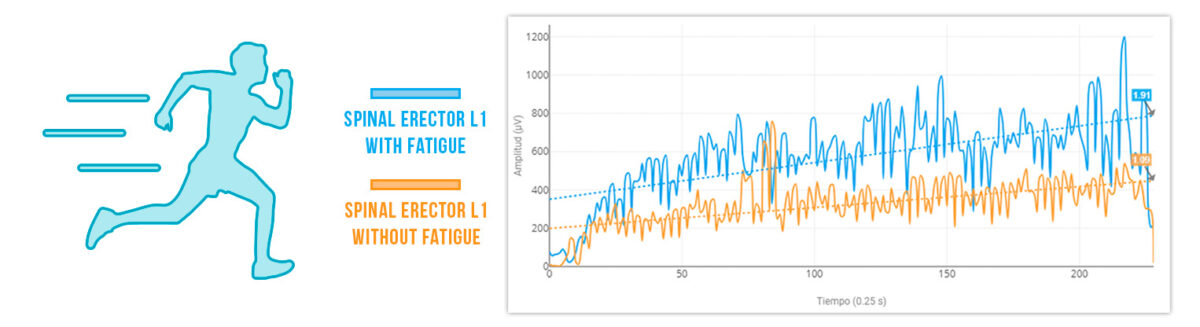
The left spinal erector fatigues twice as much as the right erector to perform the same task.
3. Poor Neuromuscular Function Leading to Faulty Movement Mechanics
This may indicate neuromuscular discoordination where nerve impulses are not effectively directed to the muscle.
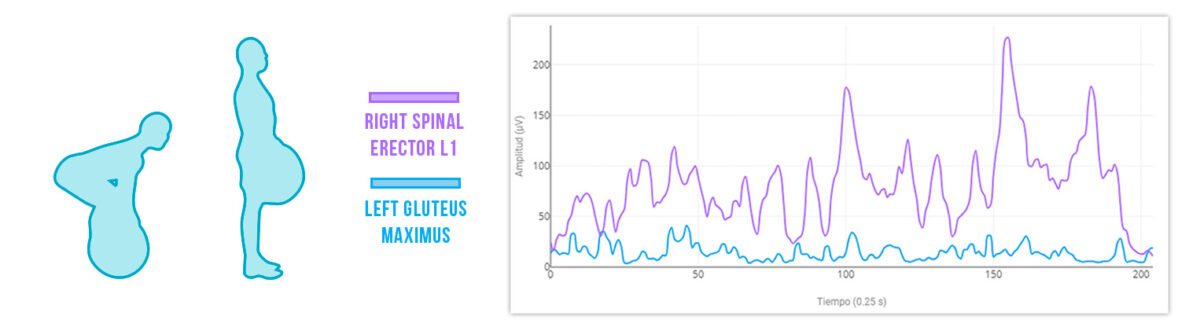
In this deadlift example, you can quickly identify:
🔹 Spinal erector: High activity indicates excessive reliance on this muscle for lifting.
🔹 Gluteus maximus: Low activation during a movement that should heavily engage it suggests it is not being properly recruited.
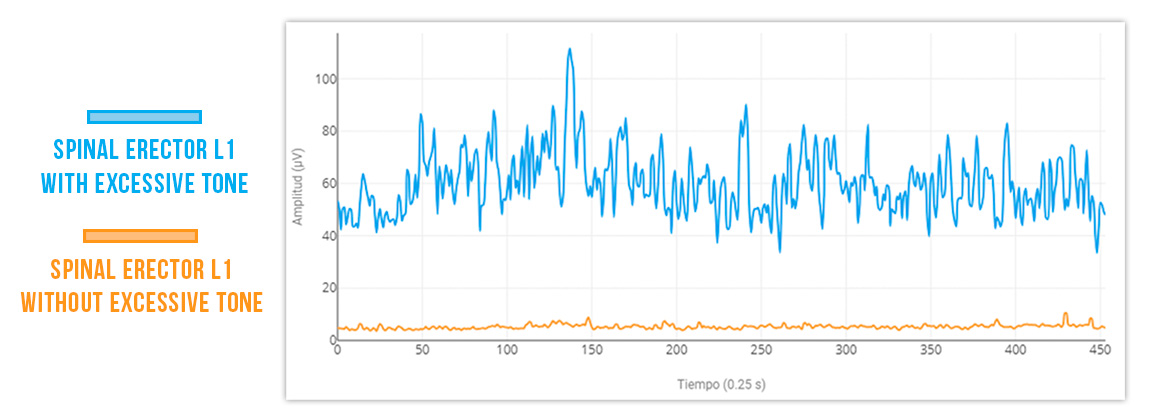
4. Altered Resting Muscle Tone
A muscle analysis can reveal an altered activation pattern that arises as a response to pain.
For example, prolonged and continuous muscle contraction as a response to pain may become evident.
5. Validating the Effectiveness of Therapeutic Interventions
By comparing EMG data before and after therapeutic interventions, you can assess whether there is an improvement in muscle activation patterns, indicating a positive response to treatment.

Notice how the yellow bar representing the gluteus maximus has increased, demonstrating that neuromodulation has positively influenced motor recruitment.
Conclusions
In summary, lower back pain is a complex condition that continuously challenges our ability as physiotherapists to diagnose and treat effectively.
However, by integrating tools like surface electromyography, we are better equipped than ever to understand the variables underlying this common issue.
EMG not only enriches your understanding of muscular conditions but also refines your treatments, making them more personalized and effective.
For you, applying this knowledge and these techniques can mean the difference between a treatment that only manages symptoms and one that addresses key issues, facilitating lasting recovery and improving your patients’ quality of life.
Additionally, educating your patients on these concepts and providing visual data of their muscle activity will significantly enhance their commitment and adherence to treatment.
If you want full access to information about the mDurance EMG system, check it out here.
See you in the next post 🙂