Look at what happens in the gluteus medius and the spinal erectors (and why it matters)
Leg length discrepancy is one of the most underestimated factors when we talk about low back pain, gait alterations, and persistent muscular compensations.
Many patients live with small differences in leg length without knowing it… and you, as a professional, may be overlooking a key factor in understanding their pain.
Even differences as small as 5 mm can generate enough muscular adaptations to trigger:
- Overload of the pelvic musculature
- Changes in lumbopelvic mechanics
- Fatigue and compensations during gait
- Reduced performance
- Chronic low back pain
And here’s the most interesting part: not all muscles behave the same way in response to a leg length discrepancy.
In this post, you’ll learn what happens specifically in the gluteus medius and the spinal erectors, based on an analysis using surface electromyography (sEMG).
By the way, if you identify with any of these statements—I want to make more objective diagnoses, fine-tune exercises more precisely, improve patient adherence, and achieve better results in less time—
then contact us here and we’ll show you how to integrate EMG into your sessions without adding extra time.
How leg length discrepancy alters pelvic and spinal mechanics
An imbalance in leg length produces immediate mechanical changes. When one leg is shorter—even by just a few millimeters—the following occurs:
- The pelvis drops toward the shorter side (pelvic obliquity).
- The lumbar spine compensates with a lateral flexion toward that same side.
- Load distribution during gait and sporting movements is altered.
- Stress on lumbar ligaments, fasciae, and musculature increases.
A severe discrepancy isn’t necessary to change muscle activation. With just 0.5 cm, adaptations already appear.
Types of leg length discrepancy and why they affect musculature
There are two types of discrepancy:
1. Structural (true)
- A real bony difference in tibial/femoral length.
- Produces permanent changes in motor patterns.
2. Functional
- Caused by postural or muscular asymmetries.
- Can be corrected with neuromuscular treatment.
Both can alter the activation of two key muscles for pelvic and lumbar stability:
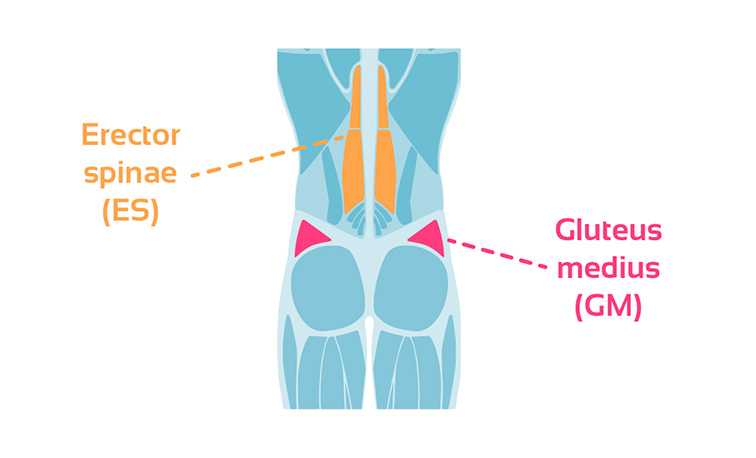
- Gluteus medius (GM)
- Spinal erector (SE)
But they don’t do so in the same way. Let’s talk data.
What electromyography shows: Gait + jump with simulated discrepancy
In this study, a group of healthy subjects performed:
- Walking at 5.7 km/h
- Countermovement jump (CMJ)
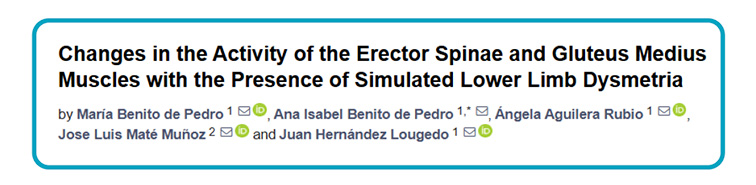
With artificial discrepancies created using insoles of 0.5 cm, 1 cm, and 1.5 cm.
This made it possible to precisely observe how muscles respond to changes in leg length.
1. What happens to the gluteus medius?
The response was clear and consistent:
Greater discrepancy → greater activation of the gluteus medius on the shorter side.
This muscle attempts to correct pelvic drop and maintain stability in the frontal plane.
This leads to:
- Increased muscular workload
- Greater effort during the stance phase
- Premature fatigue
- Increased risk of lumbopelvic overload
Clinical interpretation: A gluteus medius that works overtime will eventually fail.
And when the gluteus medius fails—what happens to the lumbar region?
2. What happens to the spinal erector?
Here’s the most interesting finding:
The spinal erector did NOT modify its activation in response to the discrepancy.
This means:
- The lumbar musculature does not compensate for the imbalance.
- The pelvis may become unstable if the gluteus medius fails.
Clinical conclusion: The spinal erector does not adapt. The lumbar spine suffers.
This combination helps explain idiopathic low back pain in patients with mild leg length discrepancies.
3. Does it affect performance? Yes—more than you think
Subjects using 5 mm insoles already showed:
- Worse jump performance (CMJ)
- Reduced force production capacity
- Poorer landing control
Muscle asymmetry affects not only pain, but also overall mechanical efficiency.
Mild discrepancy = lower performance + higher injury risk.
Clinical implications
✔️ The gluteus medius is extremely sensitive to changes in leg length
✔️ Altered gluteus medius activation may be related to low back pain, especially in patients who walk, run, or jump with repetitive patterns
✔️ Even 5 mm can change motor patterns
✔️ EMG allows you to:
- See the real activation of each muscle
- Compare healthy side vs. affected side
- Adjust treatment with precision
- Know when an insole helps… or harms
Want to learn how to assess these synergies and design precise treatments?
EMG lets you measure what the eye can’t see: compensations, deficits, overloads, and altered motor patterns.
If you want to:
- Make more objective diagnoses
- Fine-tune your exercises precisely
- Improve patient adherence
- Achieve better results in less time
Talk to us and we’ll show you how to integrate EMG into your clinical practice.