Breathing is one of the body’s most automatic movements, yet also one of the most easily disrupted by pain, stress, or respiratory dysfunction.
In many patients, respiratory dysfunction isn’t purely pulmonary in origin, it often stems from poor muscular coordination.
This is where surface electromyography (sEMG) becomes invaluable: it allows you to evaluate in real time which muscles are actually working during breathing, whether there’s insufficient diaphragmatic activation, or if the accessory muscles are overcompensating.
Understanding these patterns enables you to identify the neuromuscular cause of dysfunction, retrain breathing mechanics, and improve both respiratory function and postural control.
👉 Want to learn how to implement EMG in your respiratory assessments?
Write to us here and discover how mDurance technology can help you analyze and retrain your patients’ breathing with scientific precision.
What You Can Analyze With EMG in Breathing
Surface EMG allows you to assess three key aspects:
1. Respiratory Muscle Activity
You can record activation of both primary and accessory respiratory muscles, including:
- Diaphragm: main inspiratory muscle.
- External and internal intercostals: stabilize and expand the rib cage.
- Scalenes and sternocleidomastoids (SCM): act as accessory muscles, active during forced inspiration or compensatory patterns.

2. Muscle Compensations and Activation Deficits
A well-performed EMG reveals whether your patient is breathing diaphragmatically or thoracically, whether there’s scalene hyperactivity, or if the SCM dominates over the diaphragm.
3. Re-education of the Respiratory Motor Pattern
Using real-time biofeedback, you can visually show patients their muscle activation pattern and teach them how to relax or engage the correct muscles.
One of the most common errors in respiratory EMG assessment is incorrect electrode placement. This can create signal noise, inconsistent data, and make it impossible to compare results between sessions or with other studies.
Example:
Placing diaphragm electrodes too low may capture abdominal activity, while placing them too lateral can pick up interference from the serratus anterior.
The key is positioning the electrodes according to each patient’s functional anatomy. For reliable, clinically meaningful data, follow these anatomical references:
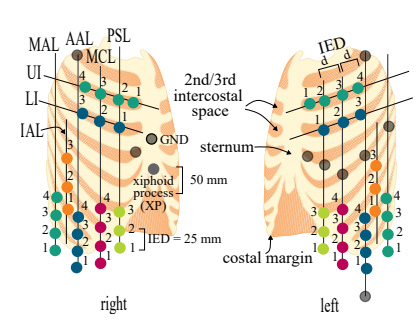
Diaphragm
Place electrodes along the midclavicular lines, approximately 2.5 cm above the costal margin. This placement ensures accurate recording of diaphragmatic activity without interference from abdominal muscles.
Intercostals
Position electrodes along the parasternal line in the second intercostal space. Adjust slightly medial or lateral depending on patient morphology.
Sternocleidomastoid (SCM)
Place electrodes on the muscle belly, at one-third of the distance between the sternum and the mastoid process. This avoids interference from the scalenes and improves signal clarity.
✅ Example of a Normal Respiratory Pattern
In a functional breathing pattern, activation follows this order:
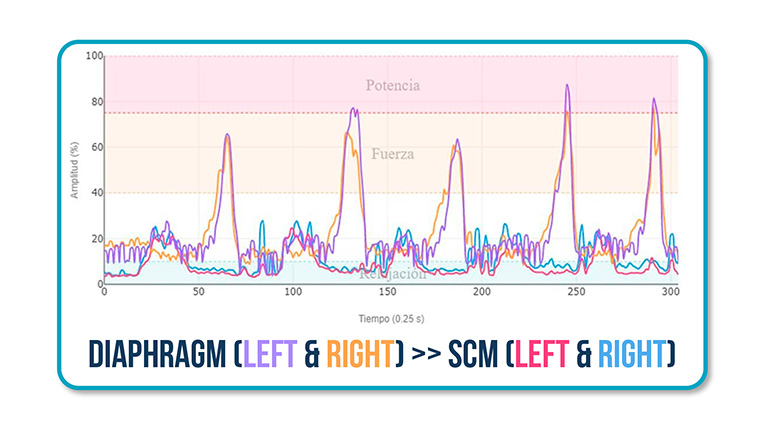
✔️ Left and right diaphragm >> Left and right SCM
This means that breathing originates from the abdomen, with minimal cervical involvement, an efficient, compensation-free pattern.
❌ Clinical Example: Accessory Muscle Compensation
A typical dysfunctional pattern seen in clinic occurs when the SCM dominates over the diaphragm:
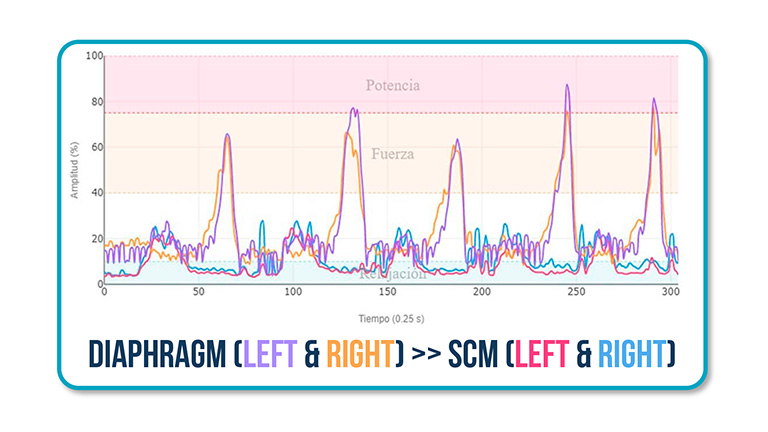
❌ Left and right SCM >> Left and right diaphragm
This indicates the patient is relying on accessory muscles to breathe, which can cause cervical stiffness, dyspnea, and thoracic discomfort.
Clinical Implications
Surface EMG is not only a diagnostic tool, it’s also ideal for monitoring treatment progress.
If you work in respiratory physiotherapy, these are the contexts where EMG provides the greatest value:
- Functional or restrictive respiratory dysfunctions.
- Cardiopulmonary rehabilitation, where assessing muscle efficiency is key.
- Patients with mechanical ventilation or post-COVID recovery, where diaphragm retraining is essential.
Additionally, in general physiotherapy, EMG can help correct altered breathing patterns that interfere with core stability and global biomechanics.
Conclusions
Applying surface EMG to respiratory assessment allows you to:
✅ Precisely identify abnormal respiratory motor patterns.
✅ Objectively evaluate diaphragm and accessory muscle function.
✅ Make clinical decisions based on objective data and personalize treatment.
Integrating it into your sessions means shifting from subjective observation to quantifiable evidence, elevating both your clinical practice and your patients’ confidence in their treatment.
See you in the next post 🙂